Doctors: Should you antibody test?
As the COVID-19 pandemic rolls on, it is important to know what kind of testing should be performed and when it is useful. Otherwise, doctors may later lack important medical information about their patients.
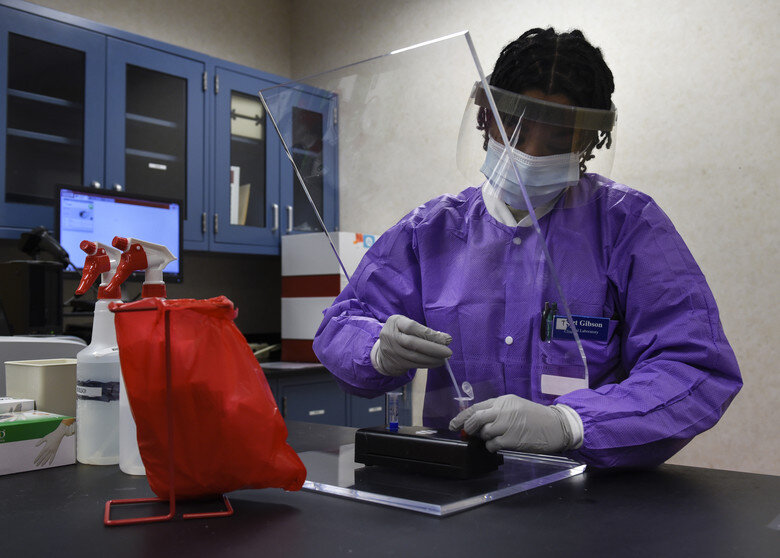
As the COVID-19 pandemic rolls on and increased wide-spread testing becomes available nationwide, antibody tests will become widely available at testing sites, urgent cares, and emergency rooms. Should you provide these tests for your patients ? What information will they provide? Are they worth doing? Here are some things to consider.
First, it is important to understand that antibody (serology) tests are not stand-alone diagnostic tests! If an individual starts having a fever and cough, and runs over to the nearest drive-up testing site that only offers antibody testing, this individual would need to drive away and find a site that offers nasal swabs (molecular tests). With that being said, the viral nasal swab PCR tests, which are the diagnostic “Gold Standard”, may have up to a 20-50% false negative rate. This means that 1 in 5 individuals who truly have the disease are not caught by these nasal swab tests, according to a Johns Hopkins meta-analysis.
If an antibody test with high sensitivity is run concurrently with a viral test, a positive IgM/IgG antibody test would suggest a recent onset coronavirus infection, and can be positive as early as a day post symptom onset in some patients. This may provide for greater confidence that a negative nasal swab test result is truly negative versus a false negative, even in the acute phase of disease, helping to identify those individuals with disease whom otherwise would think they are virus-free and continue to spread disease.
Even antibody tests with the highest sensitivity would miss some patients who have disease as antibody titers within the first week may be too low to detect with point-of care antibody tests in some patients, but not all. A clinician should use their best judgment based on the patient medical history and physical exam to determine, in the acute setting, whether or not they need to draw any blood for labs, including a serology test.
If a patient is greater than seven days out from symptom onset, it is important to know that at this point, the accuracy of nasal swabs has declined even more, and that the amount of antibodies have increased in the blood, so it would be important to administer both the nasal swab and an antibody test. If a patient is more than two weeks out from symptom onset, in most patients an antibody test alone would allow you to determine whether they have had COVID-19 except for in those who are immunocompromised or have an immune disorder. Administering a nasal swab test will have a very high rate of false negatives, much higher than an antibody test.
Antibody tests also help to identify those who are asymptomatic, as well as those who are symptomatic but never get tested due to mild symptoms. A recent epidemiological study from Spain showed that 1/3 of the greater than 61,000 cohort in their study were asymptomatic and almost 20% of those who were symptomatic never received testing. Seroprevalence studies here in the U.S. have similar findings with one study in California showing that the reported number of cases is as much as 55-fold lower than the actual number of infections.
Why is this important? In order to understand how deadly this new disease is, the infectious fatality rate (IFR) must be known. That is, the proportion of infected people who will die as a result of this disease, including those who don't get tested due to mild or no symptoms. If those detected are a smaller proportion than those actually infected, our infectious mortality rate will be much higher than truly expected. This would give false implications of the scale of this pandemic and skew the responses of governments and individuals towards overreaction nationwide, which could cause tremendous physical and mental harms from the overuse of public health interventions like lockdowns and social distancing, as well as cause extreme financial and economic strain. On the other hand if the IFR is calculated too low, this could lead governments and individuals to under-react, causing increased loss of lives and overburdening of our hospitals and hospital staff. It is important to get the IFR right within your specific region and amongst varying demographics.
Finally, how will we truly understand the future relationship between SARS-CoV-2 antibodies and immunity from COVID-19 reinfection if we miss the majority of those infected initially? How likely is COVID-19 reinfection for people with and without detectable SARS-CoV-2 antibodies? This will be hard to accurately assess with many individuals remaining undetected for both disease and antibodies. As this pandemic rolls into later parts of the year, will a COVID-19 infection be a primary infection or a reinfection? If there are individuals truly being re-infected, what does this tell us about the possible efficacy of vaccinations? We don't have enough information from scientific studies to provide the answers to these questions, but once you know who has had COVID-19 within your patient population, you will be able to also know later whether it is a reinfection or a primary infection.
If there are enough reporting antibody test results, doctors will have the information they need within their communities, and will be better able to advise, educate, and advocate for their patients, communities, and government leaders. Active and passive surveillance are so important. We cannot wait until the pandemic is over to begin antibody testing or seroprevalence studies. Understanding COVID-19 disease transmission and deadliness is limited if our diagnostic testing is only able to find those with symptoms some of the time, those without symptoms probably even less of the time, and those who have had symptoms and won't get tested, ever. Antibody testing can help with detection within each of these groups.
References:
Antibody responses to SARS-CoV-2 in patients of novel coronavirus disease 2019
Profiling Early Humoral Response to Diagnose Novel Coronavirus Disease (COVID-19)
COVID-19 Antibody Seroprevalence in Santa Clara County, California
Seroprevalence of Antibodies to SARS-CoV-2 in 10 Sites in the United States, March 23-May 12, 2020
Clinical and Immunological Assessment of Asymptomatic SARS-COV-2 Infections
Contact Us for More Information
If you have any questions or would like more information about antibody testing or the antibody tests we supply, feel free to submit your information below and we’ll reach out to you.
What qualifications and instruments do I need to perform antibody testing?
There are different types of COVID-19 antibody tests, each requiring different qualifications and instruments to run. If your clinic, hospital, or lab is considering performing its own antibody testing, here is a breakdown of the types of tests, qualifications, and instruments required to run them so you can make the right decision.
Read time: 3 minutes
There are different types of COVID-19 antibody tests, each requiring different qualifications and instruments to run. If your clinic, hospital, or lab is considering performing its own antibody testing, here is a breakdown of the types of tests, qualifications, and instruments required to run them so you can make the right decision for your organization.
Levels of Laboratory Certifications
All laboratories that perform diagnostic testing on human samples must be registered and certified under the Clinical Laboratory Improvement Amendments of 1988, a set of federal regulations commonly know as CLIA. Some tests require more care and skill to perform and can only be run by laboratories with highly-trained personnel. Other tests are relatively simple to perform and can be run by less-skilled individuals. Each diagnostic test is given a clearance level by the FDA ranging from Waiver to High Complexity. Here is a breakdown of the different levels of certification as they relate to various COVID-19 tests.
1. Waiver
Waiver is the lowest level of clearance required to perform a test. Most clinics apply for and receive this level of clearance. There are currently 5 tests that have been granted waiver status by the FDA. They require a sample to be collected by a swab and then placed in a specialized instrument for analysis. Turnaround times typically range from 30 minutes to a few hours. Some of these tests have not demonstrated as high of sensitivity or specificity as other diagnostic tests, but are much easier to perform because they do not require complicated laboratory processing.
We expect to see more tests granted waiver status over time, including antibody tests. Currently, there are no antibody tests granted Waiver status by the FDA.
2. Microscopy
This certification primarily applies to laboratories that perform microscopy on patient samples — i.e. looking at a sample under a microscope. This does not apply to COVID-19 testing.
2. Moderate Complexity
Moderate complexity tests require a higher level of skill and training to perform correctly. They must be run under the direction of an MD or PhD with clinical laboratory training and laboratory technicians and other staff must meet certain education and training requirements.
There are about 25 tests that have been granted authorization to be performed by moderate complexity labs. These include about 15 antibody tests and 10 swab tests. Some antibody tests still require specialized analyzers to obtain results, as do the swab tests, but they are generally easier to perform than the “gold standard” diagnostic swab tests, which are classified as high complexity.
3. High Complexity
High complexity tests require the highest level of skill and training to perform correctly. They must be run under the direction of an MD or PhD with extensive clinical laboratory training. Laboratory technicians and other staff must also meet more stringent education and training requirements to perform testing at this level.
There are about 80 tests that have been granted authorization for processing by high-complexity labs. These are the vast majority of the “gold standard” swab tests being performed throughout the country. Swab samples are collected by a qualified healthcare provider, placed in a tube with a stabilizing media, and transported on ice to a high-complexity CLIA lab for processing.
There are also nearly 200 antibody tests that are listed on the FDA’s notice to distribute list. These tests do not have EUA authorization and must be run in high complexity labs by default. That list can be found here under the dropdown entitled “Q: What commercial manufacturers are distributing serology test kits under the policy outlined in Section IV.D of the Policy for Coronavirus Disease-2019 Tests?”
Applied Biosystems 7500 Real-Time PCR System used to run some COVID-19 diagnostic tests. Photo credit: Wikimedia Commons
Processing of the gold standard diagnostic tests takes place in a controlled environment to minimize sample contamination and cross-contamination, involves the use of extraction reagents to purify RNA from the samples, and then processing of the samples by a PCR instrument that utilizes thermo-cycling and fluorescence analysis to amplify and detect the genetic material of the virus. Total processing time is around 3 hours. Though there is one authorized PCR test can be run in about 30 minutes.
Types of Antibody Tests
Not all antibody tests are the same. In fact, tests vary widely in required skill levels required to perform and detection methods used. Some tests can be performed in moderate complexity labs while others must be performed in high complexity labs. Some tests require special instruments to obtain results, and others give a simple visual readout, like a pregnancy test. The advantage of more complicated tests is that they usually give more accurate results. However, that is not always the case. Here is a breakdown of the four main types of antibody tests current authorized by the FDA.
1. Lateral Flow Assay
Lateral flow assays are the simplest type of antibody test. They require a drop of blood and a couple drops of buffer to be placed onto a test cassette, followed by a 10-15 minute wait, and then visually reading the results window. The presence or absence of certain test lines determine a positive or negative result. There are currently 4 authorized lateral flow tests. We supply two of them.
2. Chemiluminescence Assay
Chemiluminescence immunoassays are similar to lateral flow assays except they require a special instrument to detect the chemiluminescence. There are currently 9 authorized chemiluminescence tests. Most can be run by moderate complexity labs.
3. Fluorescence Assay
Fluorescence immunoassays are similar to chemiluminescence tests except they detect fluorescence instead of chemiluminescence, which also requires a special instrument. There is currently 1 authorized fluorescence test. Most can be run by moderate complexity labs.
4. Enzyme-Linked Immunosorbent Assay (ELISA)
ELISAs are the most complicated type of antibody test to run. They require high complexity certification, careful preparation of samples, special instruments, and several hours to obtain results. There are currently 5 authorized ELISA tests.
What are the differences in accuracy of the tests?
According to the FDA’s serology test validation program results, on average, ELISA and chemiluminescent assays, which require special analyzers, outperformed lateral flow assays by about 0.5% sensitivity and specificity. However, some of the lateral flow assays performed as well or better than some of the ELISAs and chemiluminescence assays. All of the EUA authorized antibody tests are within about 1% accuracy of each other.
The advantage of the lateral flow assays are that they require no special equipment or training and are likely to eventually obtain Waiver status, which means they can be run at point-of-care by most healthcare personnel. They are also the least expensive.
Conclusion
If you are a moderate complexity lab without special analyzers, a highly accurate lateral flow assay is your best option. If you have an analyzer, or high complexity certification, and would like to improve accuracy, you should consider chemiluminescence or ELISAs. However, check the sensitivity and specificity clinical validation data because there are some exceptional lateral flow assays that outperform more complicated tests.
If you have any questions or would like help setting up antibody testing at your lab, clinic, or other organization, please let us know.